With the release of the COVID-19 vaccination to pharmacies for distribution, we have received a lot of phone calls on how to bill the insurance. Isaac Nielson, one of our three-year support veterans, put together the following “How-To” document for this purpose.
Isaac started with FSI in 2018. After studying and living in Seattle for a few years, we were fortunate to be able to add Isaac, and his unique qualifications, to our team. Isaac is a highly dedicated support technician who sticks with a problem from start to finish. Not only will he resolve a problem, but he will also learn how and why the problem occurred so he can better understand the fix. His knowledge of pharmacy is also very diverse. Whether you need assistance with your hardware, software, or networking, Isaac is always up to the task. Don’t hesitate to allow Isaac to help you with any of your FSI needs!
This article was published by Ross Snyder – FSI Sales, Account Management, and Customer Engagement
The following documentation was provided by Isaac Nielson – FSI Technical Support
Billing to Medi-Cal:
The NDC of the drug must be the NDC of the VIAL, not the box.
This NDC will use the same CVX code as the box’s. Ensure that, if you are using FSI as a method of transmitting your vaccination scripts, the CVX code is in the correct T.P. Drug Code as set in the O, Custom Rx Data, C-[F2]: CVX/CPT Drug ID#.
In the drug’s pricing, set the AWP to $200.
*The reason for the $200 is for the maximum payout of $40.
The pharmacy that helped us become able to create this guide had the acquisition cost of $.01 set, so we do not know if an acquisition cost of $0.00 will be accepted by Medi-Cal. Any insight into whether this is possible or not is greatly appreciated and may be emailed to isaac.nielson@fsi.us.com.
Note: You will need to adjust the wholesaler pack size to match what is appropriate for the specified dispensing packsize.
During the actual billing, you will still need a Claim Clarification Code matching which dose you are administering. Additionally, you will need to provide a prior authorization number of 999999. (Six nines.)
No HCPCS or DUR codes are required.
Billing the Janssen, Pfizer, & Moderna Vaccines to Medicare Part B
Billing the Janssen, Pfizer, & Moderna Vaccines to Medicare Part B: As of 4.14.2021, there’s been an adjustment to bill to Medicare Part B. The below codes are what we currently have:Pfizer: Product# 91330 (TP. Drug Code #1); first dose: 0001A, second dose 0002AModerna: Product# 91301; first dose 0011A, second dose 0012AJohnson & Johnson/Janssen: Product# 0031A; No other codes required.These also require the specified dispensing pack size to be a “1” as in “one injection” or else the claim will be rejected. Our recommendation is to create this new profile by copying one of your drug profiles with a .5ml specified dispensing pack. DO NOT change a drug’s specified dispensing pack size to a 1 that was already set as a .5ml. Our program will warn you if this is attempted and will log whoever forces the change. The reasoning behind this is that whatever you change will affect ANY script that has been dispensed with that drug. For the Moderna & Pfizer drugs, put the Product# in the T.P. Drug Code #1 and the dose in the T.P. Drug Code #8. For the Johnson & Johnson/Janssen drug, you only need to put the product number in the T.P. Drug Code #8.Disclaimer: These values and steps are subject to change at any time and we do not currently have any examples of the Pfizer drug being successfully billed. According to the following link, it seems the Pfizer should be billed the same way as the Moderna. Link: COVID 19 Billing for NCDP MembersPlease email isaac.nielson@fsi.us.com or tamara.snyder@fsi.us.com if you have insight into billing any of these drugs. Press [ENTER] then return to the home screen by pressing CTRL+B or the home button in the upper left if you are using FSI Client. Both shortcuts function in the same way and can be used across either Client or Alphacom. An amendment will need to be made to the Third Party that we’re using to bill this drug to Part B. From the main menu press F-1 or 3-7-1-1 and pull up the Third Party’s profile. In the bracket for “Use Drug ID Number”, put an “8”. For the Qualifier put a 9.
Billing a COVID-19 Vaccination
The first step is to make sure you have your third party set up to send incentive fees, just like any other vaccination.
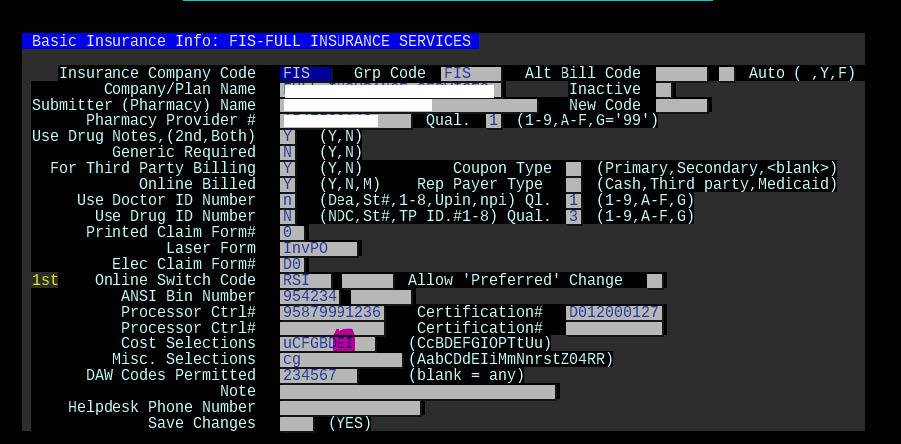
Third Party Maintenance:
Go to the Third Party Maintenance which can be reached by pressing “F” or 3-7-1-1 from the Main Menu. Enter in the code of your third party to amend.
What you’re looking for is an “E” and “I” in the Cost Selections (as highlighted in magenta below):
The next step is billing. Go back to the main menu, pull up the patient, and press “3” to start a new script. For this example, I’ll be using our friend Bobby Test and the NDC 80777027399 for the Moderna COVID19 vaccine.
Continue processing as normal. If you’re using the electronic processing for CAIR that we offer, there will be a few steps in that pathway that is in another tutorial.
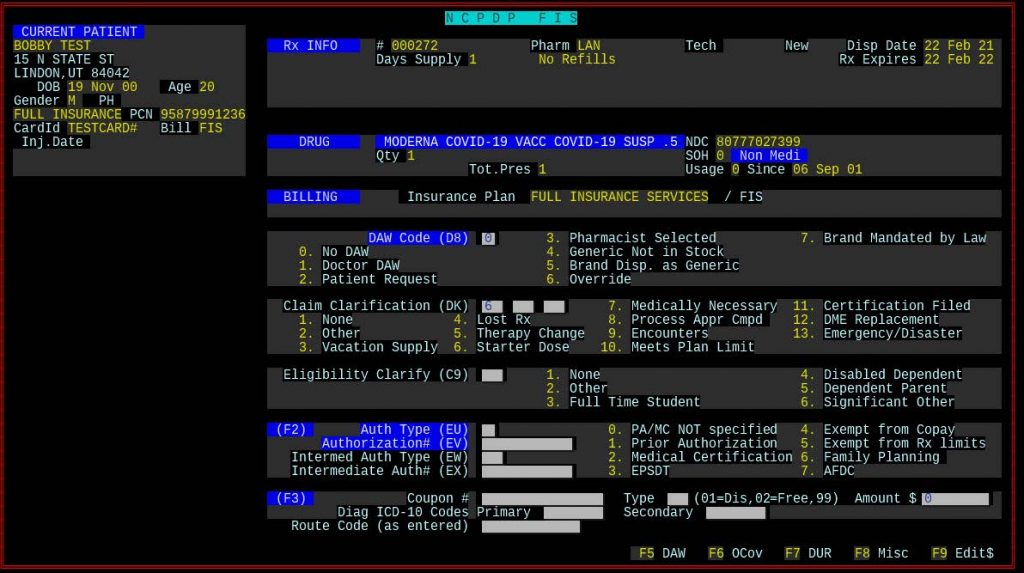
After you type “Y – Accept As Is” and hit [ENTER], stop at the screen where you can put in DAW, Claim Clarification Codes, Other Coverage, DUR Codes, etc. Press [F5] to enter the DAW/Claim Clarification portion.
For the first dose, put a “6” in the first Claim Clarification bracket as shown below:
Press [ENTER]. Now we need to add in an Incentive Amount. That’s where the “E” and “I” in the TP Maintenance’s Cost Selections comes in.
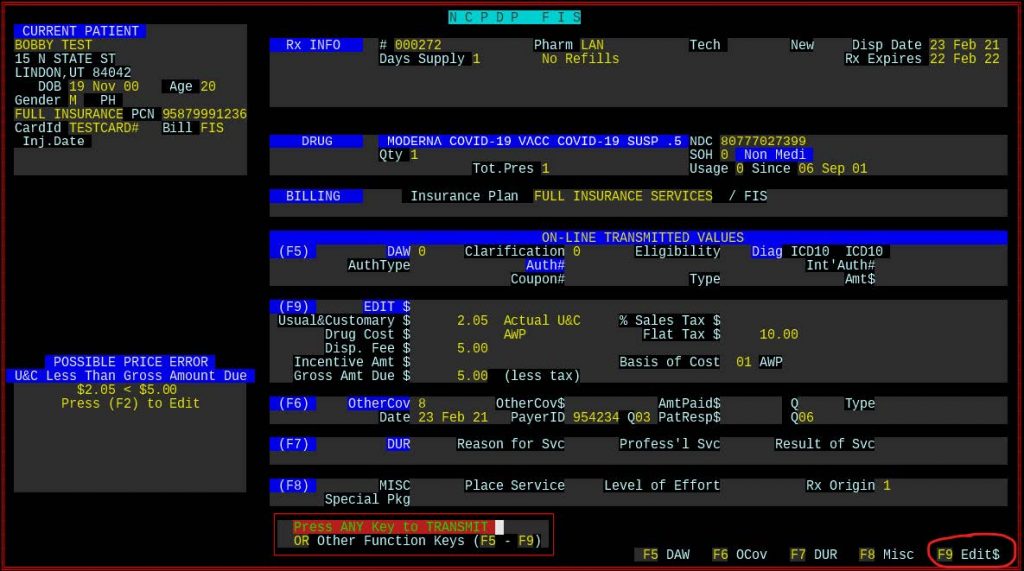
Press [F9] “Edit$” to get to the screen that will allow you to adjust the Incentive Amount.

We have no guideline as to how much to charge for an incentive amount. You may need to ask the insurance what value needs to be entered in.
NOTE: The insurance may not accept the claim unless your Basis of Cost is set to 15 to indicate that the claim is for a “Free Item”. The Basis of Cost can be found exactly to the right of the Incentive Amount field.
Press [ENTER] to save your changes, then [ENTER] again to send the claim.
Fix rejects from the insurance (if any).
If you need to see how much incentive was paid by the insurance, go to the Main Menu, pull up the script, and press “M” (More Script Functions) then “I” (Claim Log). You can then select a dispensing to view what you sent to the insurance. Press F6 to view what the insurance responded with. It should have a line that tells you how much of the incentive amount was paid.
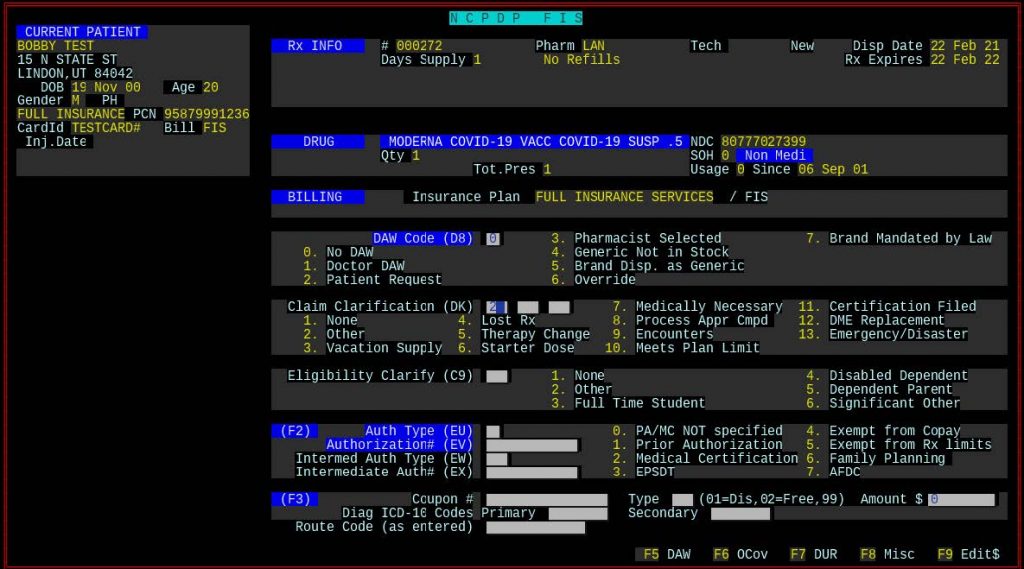
Second Dose Billing
The second dose is much like the first. The only difference is the Claim Clarification code. This time you will need a “2” in the first Claim Clarification bracket as shown below.
Press [ENTER], [F9], and enter in the Incentive Amount. Press [ENTER] and send the claim on its way.
Fix rejects from the insurance (if any).
Again, you can check the Claim Log to verify that the insurance paid you an incentive amount.
**** UPDATES ****
Look for a standard blog post for The FSI 411 in the near future, a place where you can interact with FSI and other FSI customers.
*****************************************************************************************************************************
From an FSI user:
“Just FYI first dose of Moderna is 02 in SCC field, use SCC of 06 for Moderna 2nd doses or J&J 1 dose vaccines! We’ve been billing since March 1st so have figured out a couple common issues!”
*****************************************************************************************************************************
FROM OUR FRIENDS AT Express-Scripts:
| COVID-19 Vaccine Processing Update 03.05.2021 To process COVID-19 vaccines, please submit claims in accordance with the instructions set forth in the Express Scripts Provider Manual with the below additional information. Submission Clarification Codes to Indicate First or Subsequent Fill COVID-19 vaccine claims require a Submission Clarification Code (SCC) in NCPDP field (420-DK) to indicate whether the claim is for an initial dose, a final dose, or the only dose of a vaccine series and for applicable clinical safety edits to be invoked. Missing SCCs will cause claims to reject. For multi-dose COVID-19 vaccines, the following Submission Clarification Codes must be used: Initial dose: 02 Second dose: 06 For single-dose COVID-19 vaccines, the following Submission Clarification Code must be used: Single dose: 06 Medicare Part D Reminder All Medicare Part D and Medicare Advantage claims for COVID-19 vaccines must be processed to the Original Medicare Part B Fee-For-Service by submitting to the Medicare Administrative Coordinator. Medicare Part D claims that are submitted incorrectly may cause one of the following rejects: NCPDP Reject A5 (Not Covered Under Part D Law) NCPDP Reject A6 (This Product/Service May Be Covered Under Medicare Part B) NCPDP Reject 816 (Pharmacy Benefit Exclusion, May Be Covered Under Patient’s Medical Benefit) If you need a member’s specific prescription processing information or other help with a claim, please visit our Pharmacist Resource Center at https://prc.express-scripts.com. Thank you, Provider Outreach Team Express Scripts |
| Express-Scripts.com One Express Way St. Louis, MO 63121 |
| © 2021 Express Scripts. All Rights Reserved. |






If you can comment on this post and help someone having an issue, go for it!